Cataract surgery is a common and generally safe procedure, but like any surgery, it does come with some risks. Being aware of the potential complications can help you weigh the pros and cons and make an informed decision about whether cataract surgery is right for you.
Infection
One of the most common risks of any eye surgery is infection. Cataract surgery creates an open wound on the eye that can allow bacteria to enter and cause an infection. The reported rate of endophthalmitis (infection inside the eye) after cataract surgery is around 0.1% to 0.3%. Symptoms of infection include eye pain, swelling, redness, blurred vision, and discharge. Infections must be treated immediately with antibiotic eye drops or injections to prevent permanent vision loss.
Bleeding
Though rare, bleeding inside the eye (hyphema) can occur during cataract surgery. The risk is higher in patients who take medications that interfere with clotting, such as aspirin or warfarin. Signs of bleeding include blood in the clear gel inside the eye, increased eye pressure, and blurred vision. Mild bleeding often resolves on its own, but severe bleeding may require additional surgery to drain the blood and reduce eye pressure.
Retinal detachment
In about 0.5% to 1.5% of cases, the retina can become detached during cataract surgery. This occurs when the thin lining at the back of the eye lifts away from underlying tissue. Symptoms include sudden flashes of light, shadowy curtain over the field of vision, and blurred vision. Retinal detachment is a medical emergency that can lead to permanent vision loss if not treated promptly with laser therapy or additional surgery.
Swelling of the cornea
The cornea is the clear, curved outer layer of the eye. In some cases, it can become swollen and cloudy after cataract surgery, resulting in blurred vision. Mild swelling is common and usually resolves within a few days. But severe swelling called corneal edema can require further treatment with eye drops.
Dropped lens fragment
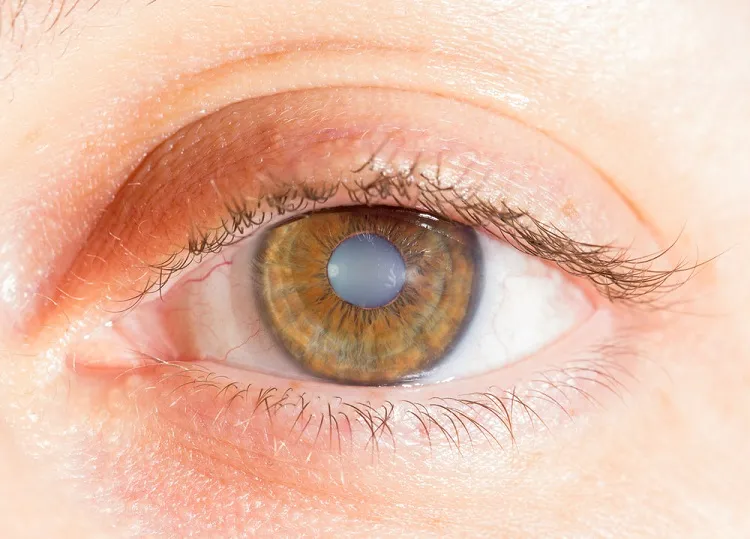
During cataract surgery, the eye’s cloudy natural lens is broken up using ultrasound and suctioned out. In very rare cases, a small piece of the lens can fall down into the back of the eye. This can cause inflammation and require additional surgery to retrieve and remove the fragment.
Dislocation of the new lens
After the old lens is removed, a clear artificial lens is implanted into the empty capsule to restore focusing power. In less than 1% of surgeries, the new lens becomes decentered or dislocated. This can result from weak capsular support or surgical complications. Additional surgery may be needed to reposition or replace the artificial lens.
Abnormal healing of the corneal incision
Cataract surgery is done through a tiny incision on the cornea. While most incisions heal within several weeks, abnormal healing can cause inflammation, hazing, astigmatism, or glare and halo effects around lights at night. If this occurs, the surgeon may recommend using steroid eye drops to control inflammation and speed healing.
Worsening vision
While most cataract surgeries successfully improve vision, in rare cases vision can become worse after the procedure. Potential causes include surgical complications, bleeding, swelling, infection, retinal detachment, or a dislocated lens. Refractive errors, such as nearsightedness or astigmatism, can also cause trouble seeing after surgery in some cases. Additional treatment and follow-up care can often improve vision.
Need for glasses
While cataract surgery aims to reduce or eliminate the need for prescription eyeglasses, some patients still need glasses for certain tasks after surgery. Glasses may be required for reading, driving, computer work, or seeing details up close. Many people still need sunglasses after cataract surgery to protect their eyes outdoors. Your ophthalmologist can advise you on your expected need for glasses after surgery based on your eye anatomy and surgical plan.
Double vision
Seeing double is possible but very uncommon after cataract surgery. Potential causes include swelling, a dislocated lens implant, or preexisting muscle problems around the eyes. In most cases, double vision is temporary and improves within days or weeks as healing progresses. Occasionally, surgery or prism lenses may be required to correct double vision that persists.
Anesthesia risks
Cataract surgery is typically done using local anesthesia with sedation or general anesthesia. As with any surgery requiring anesthesia, potential risks include allergic reactions, breathing problems, nausea and vomiting, and very rarely heart or lung complications. Your anesthesia provider will take all necessary precautions to minimize risks based on your medical history.
While significant complications from modern cataract surgery are uncommon, being aware of the risks can help you make an educated decision. Discuss any specific concerns and your personal risk profile with your ophthalmologist to understand the benefits and risks in your situation. With an experienced surgeon using state-of-the-art techniques and equipment, cataract surgery can safely and effectively restore vision for the vast majority of patients.
Factors That Influence Risk
Several factors can influence the risk of complications from cataract surgery, including:
- The surgeon’s experience and skill
- Your overall eye health
- Pre-existing eye conditions
- The type of intraocular lens used
- Your general health and medical history
Minimizing Risks
While some risks are inherent to cataract surgery, there are steps you and your surgeon can take to minimize them:
- Choose an experienced and skilled surgeon.
- Disclose your full medical history and any medications you’re taking.
- Follow all pre-operative and post-operative instructions.
- Attend all scheduled follow-up appointments.
- Be vigilant for any signs of infection or complications and report them promptly.
FAQ About Risks of Cataract Surgery
What is the most common complication of cataract surgery?
The most common complication is posterior capsule opacification, which occurs when the back part of the lens capsule becomes cloudy months or years after surgery. This can blur vision again but is easily corrected with a laser procedure.
How long does it take to heal after cataract surgery?
Most patients see improved vision within a few days after surgery. Complete healing of the eye and stabilization of vision can take 4-6 weeks. Use medication as directed and avoid rubbing your eyes during the healing process.
Can cataract surgery cause blindness?
Permanent severe vision loss or blindness after cataract surgery is extremely rare. But there are small risks of serious complications like infection, bleeding, or retinal detachment that could lead to blindness if not treated promptly.
When should I see a doctor after cataract surgery?
Contact your ophthalmologist right away if you have increasing eye pain, discharge, swelling, redness, or sudden changes in vision like new floating spots. These could indicate a serious complication needing immediate treatment. Routine follow-up visits are also important.
How do I reduce swelling after cataract surgery?
Use anti-inflammatory eye drops as prescribed by your surgeon to prevent excessive inflammation. Limit straining or bending which can increase eye pressure. Apply cool compresses and avoid rubbing your eye. Elevate your head with pillows when resting. These tips can help reduce postoperative swelling.
What are the signs of an eye infection after surgery?
Increasing eye pain, light sensitivity, redness, discharge or fluid leakage from the eye, and impaired vision can signal an eye infection. You may also have blurred vision, swelling and heat around the eye. See an ophthalmologist immediately at the first signs of infection.
Contact us at 9211722214 to schedule an appointment for your caataract surgery. We are honored to offer seamless eye care services because we truly think that “every eye deserves the best.”